Newsletter 2:2013
May 1, 2013
We recently reported a strong association between the number of HLA mismatches and the
rate of death with a functioning graft in kidney transplant recipients. Death from infection
and cardiovascular disease was affected by the HLA match whereas death from cancer was
not (Am J Transplant 2012; 12: 3031-8). The next logical step was to examine whether these
findings also applied to heart and liver transplants. The CTS, thanks to your generous
support, has data available that allow the analysis of this question. One must bear in mind, of
course, that since the rate of death is relatively low, very large patient numbers are necessary
to perform a meaningful analysis of the complex factor HLA. The numbers of heart and liver
transplants contained in the CTS database are far smaller than the number of kidney
transplants, but we believed this would be worth exploring.
An initial analysis indicated that the definition of ‘death from cardiovascular causes’ was
problematic for heart transplant recipients because graft failure could not be distinguished
from death due to reasons unrelated to the graft. As a result, the findings were not meaningful
in the heart transplant population or, indeed, in liver transplant recipients. Death from cancer,
however, was shown to be unaffected by the HLA match as reported previously in the kidney
transplant recipients.
The analysis of death from infection proved interesting. Although less striking than the data
from kidney transplants, we observed an association between the number of HLA-A+B+DR
mismatches and the rate of death from infection in both heart and liver transplant
recipients.
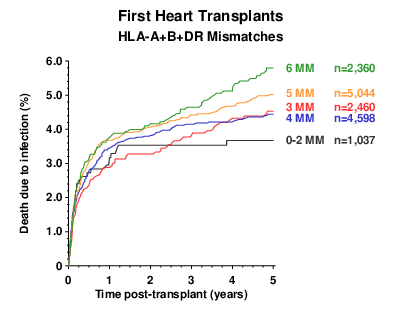
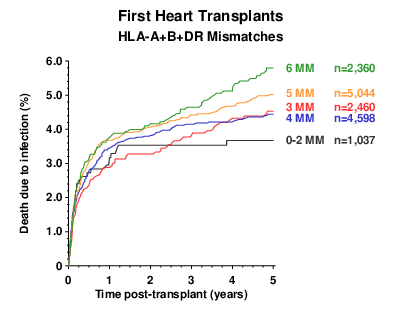
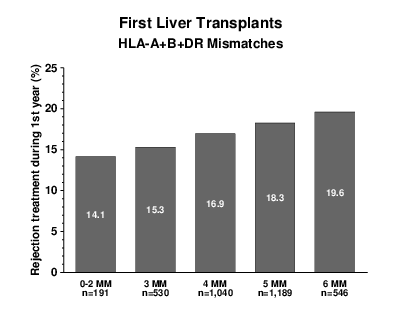
Figure 1
Figure 1 shows the rate of death from infection during the first 5 post-transplant years in
heart transplant patients. We had to combine transplants with 0, 1 or 2 mismatches because,
since hearts are not prospectively matched according to HLA, the number of well-matched
heart grafts is relatively small. On this basis, the correlation between the number of HLA
mismatches and death from infection reached statistical significance (log rank trend analysis:
p=0.015).
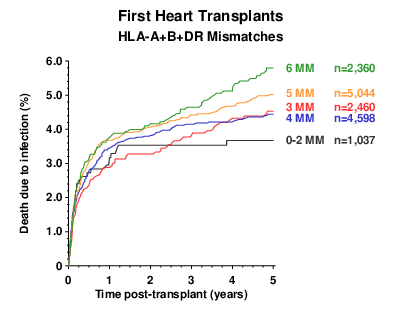
In searching for an explanation of this effect, we analyzed the rate of rejection treatment
during the first post-transplant year. As information on rejection therapy is collected in the
CTS for patients with a functioning graft at the end of year one, rejection episodes that
occurred in patients who lost their graft during the first year are not captured in the database.
The association between treatment for rejection, based on the information on patients with a
functioning graft at one year, and the number of HLA-A+B+DR mismatches in heart
transplant patients was not striking, but it was statistically significant (Figure 2, p=0.008).
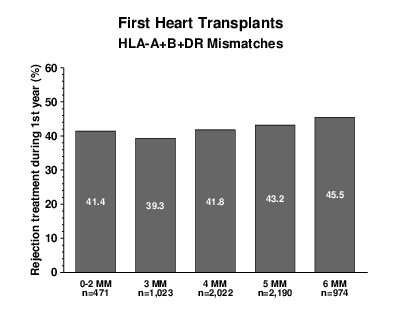
Figure 2
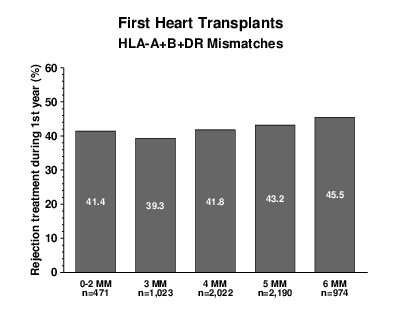
The corresponding results for liver transplants from deceased donors are shown in Figures 3
and 4. Here again, although the curve for 5-mismatch grafts did not fit perfectly, the
association between death from infection and the number of HLA-A+B+DR mismatches
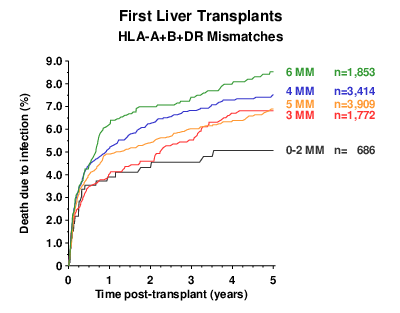
was significant (Figure 3, p=0.034). Likewise, the rate at which rejections were treated
during the first post-transplant year (as documented for patients with a functioning graft at
year one) correlated significantly with the number of HLA mismatches (Figure 4, p=0.017).
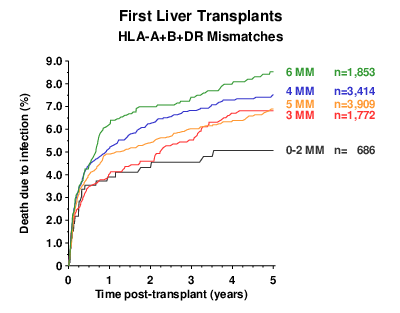
Figure 3
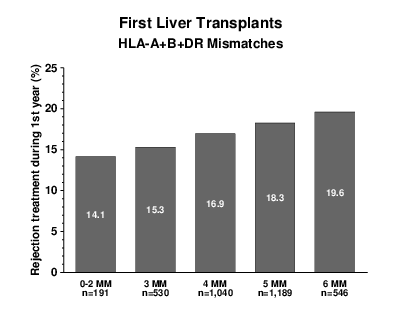
Figure 4
Together, these data show that even in heart and liver transplants, in which the effect of
HLA matching on graft outcome is not nearly as well established as in kidney grafts, the rates
of rejection and recipient death from infection are still associated with the numbers of
HLA-A+B+DR mismatches. We believe that the need for more frequent and more potent
rejection treatment in patients with more HLA mismatches is a likely explanation for this
effect.
We hope you will find these findings interesting and, as always, we would like to thank you for your
outstanding commitment and support which makes this type of large-scale analysis possible.
Best wishes,
Gerhard Opelz