Newsletter 4:2016
November 1, 2016
Dear Colleague,
We dedicated this newsletter to two hotly debated topics, namely the allocation of kidneys from
elderly donors and the impact of a positive crossmatch in liver transplantation.
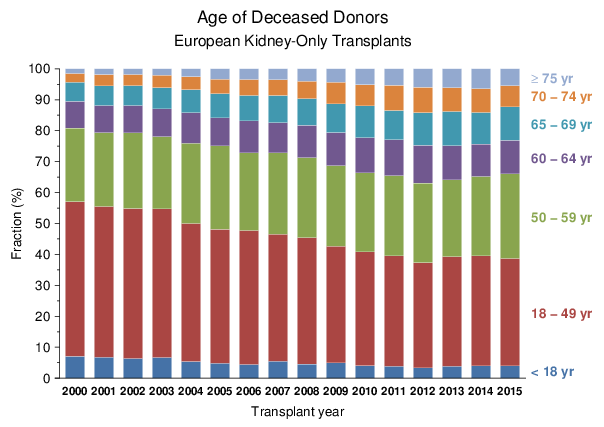
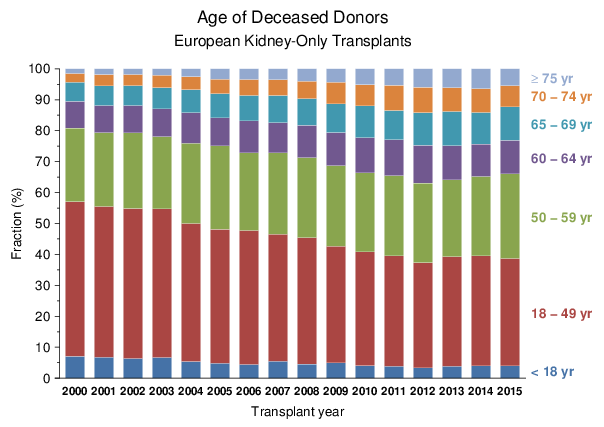
Data from European centers participating in the CTS underline the general trend that the
“donor population is continuously growing older”. As shown in Figure 1, the percentage
of ≥60 year old deceased kidney donors increased from 19.1% in 2000 to 36.9% in 2012.
Although no further increase is evident after 2012, as many as 1 in 4 of deceased donors currently
belong to the age group ≥65.
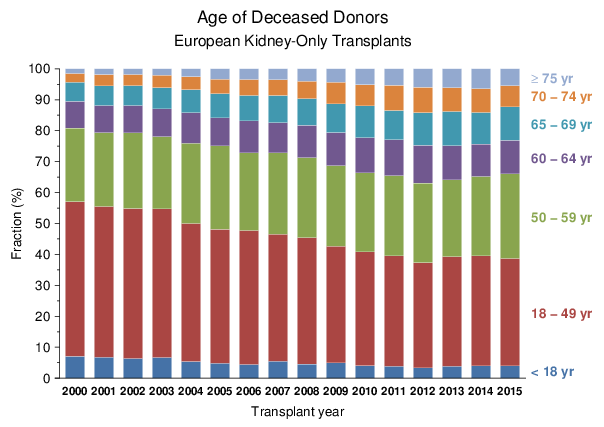
Figure 1
To enable the transplantation of “marginal organs” from elderly donors, age-matched old-for-old
allocation programs were introduced in the 1990’s. For example, in the Eurotransplant Senior Program (ESP),
organs from ≥65 year old donors are allocated primarily to ≥65 year old recipients, without
consideration of HLA matching in order to ensure a cold ischemia time as short as possible. Introduction of
ESP indirectly and markedly influenced the recipients’ age profile. The percentage of the ESP transplantations
increased from 9% in 2000 to 15.5% in 2015 (ET Annual Reports 2000 and 2015). In the CTS Newsletter 4:2015
we pointed out the changing recipient age profile and described a “striking spike at about age 65”
which cannot be attributed to the aging of the general population.
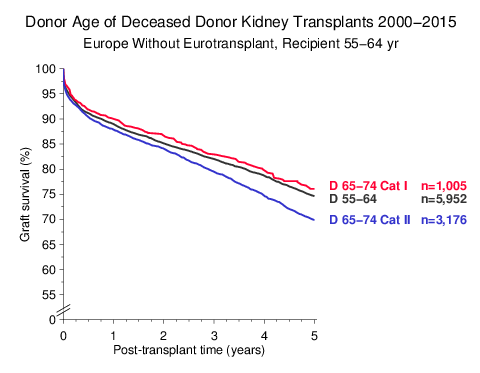
Donor kidneys obtained from elderly donors are not necessarily “marginal” organs. Hypertension, increased
serum creatinine of >1.5 mg/dl and death from cerebrovascular accident are the currently used
additional parameters to define an “Expanded Criteria Donor” in the age group 50–59. Using these
same parameters, we categorized for the purpose of this newsletter the ≥65 year old donors into two
different groups. Category I: no history of hypertension, no increased creatinine, no cerebrovascular
death, and no other reason for defining a marginal donor, such as diabetes, cancer, alcohol abuse, or cardiac
insufficiency. Category II: history of hypertension or cerebrovascular death or increased creatinine
or other reason(s) for defining a marginal donor. We then analyzed the impact of this categorization on graft
survival. To eliminate a possible influence of the ESP program, transplant centers belonging to the
Eurotransplant-region were excluded.
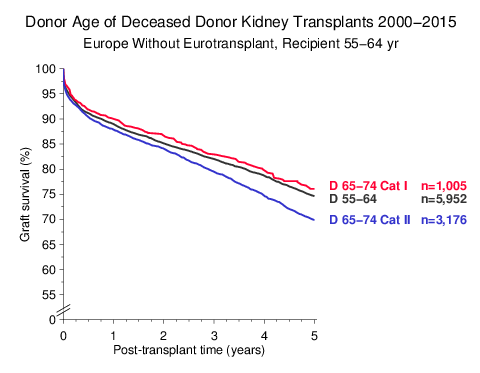
Figure 2
Figure 2 shows that transplantation of Category I kidneys from 65–74 year old donors to 55–64 year old
recipients yielded virtually equally good results as transplantation of kidneys from 55–64 year old donors
to 55–64 year old recipients. Importantly, as many as one quarter of the 65–74 year old donors belong to
Category I. Our results therefore indicate that allocation of donor kidneys from Category I 65–74 year old
donors to somewhat younger recipients aged 55–64, rather than strict old-to-old age matching, results in a
more favorable utilization of kidneys from the donor age category 65–74. In 65–74 year old recipients,
only 28% of Category I kidneys from 65–74 year old donors survived after 10 years. Almost twice as many
(53%) of these kidneys were shown to have been functional after 10 years in 55–64 year old recipients.
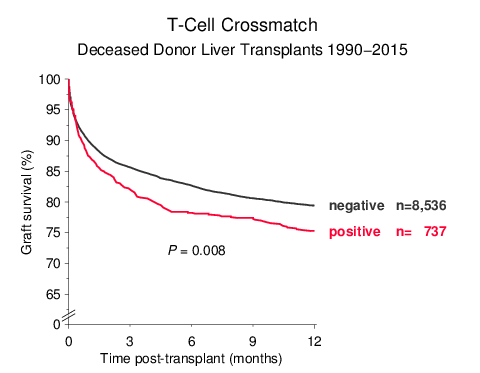
Another hot issue is whether prospective virtual or real crossmatching should be practiced in liver
transplantation. In the CTS paper “Analysis of positive kidney, heart and liver transplant crossmatches
reported to the Collaborative Transplant Study” (Hum Immunol 70:627–630, 2009) we reported that
a positive complement-dependent cytotoxicity (CDC) T-cell-crossmatch result before liver transplantation
is associated with a significantly higher graft loss. The time periods 1990–1999 and 2000–2007 were analyzed
in that paper. In the meantime, we were able to extend the analysis to the time period 1990–2015 and confirm
the previous findings (Figure 3). Already 5 months after transplantation, crossmatch-positive patients
had a significantly higher liver graft loss rate than crossmatch-negative patients (21.5% vs. 16.5%).
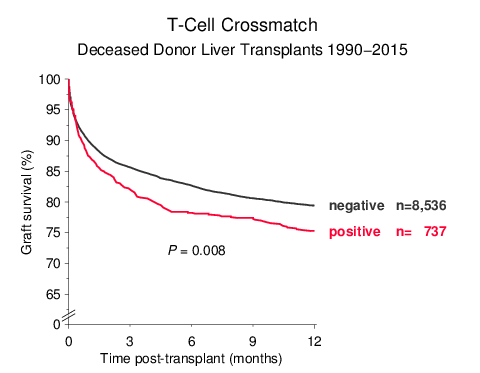
Figure 3
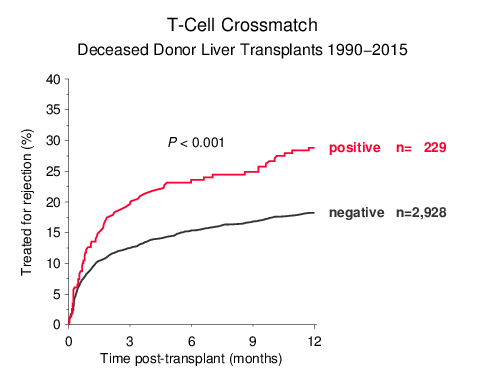
When patients with a functioning graft at year one were analyzed, the rate of treated rejections during the
first year was 10% higher in crossmatch-positive patients than in crossmatch-negative patients
(28.8% vs. 18.2%) (Figure 4).
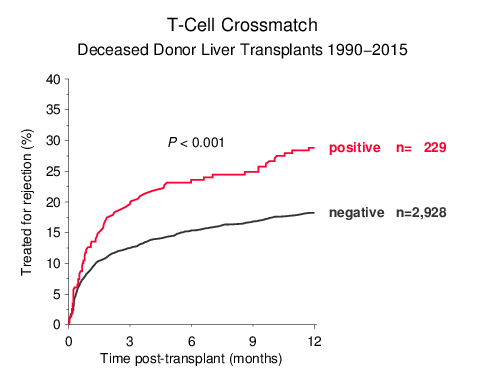
Figure 4
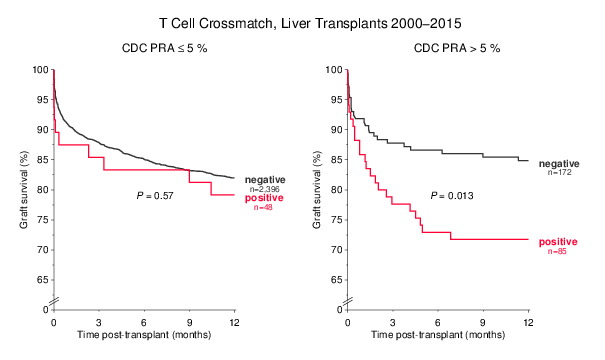
Although the rather low number of patients with crossmatch information does not allow a more detailed
analysis, Figure 5 impressively demonstrates that the T-cell crossmatch effect is still existent
in the current transplantation period from the year 2000 onwards, and is especially evident in
presensitized patients who possessed panel reactive lymphocytotoxic antibodies (PRA) prior to
transplantation.
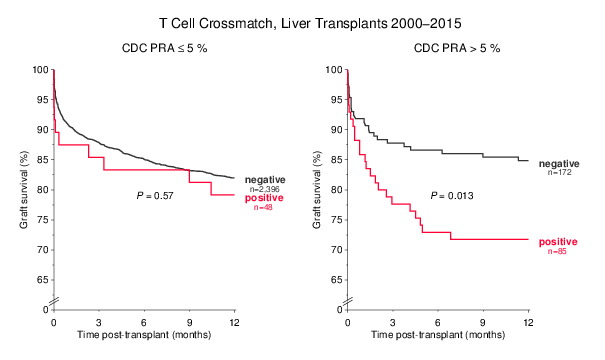
Figure 5
All 2,731 graphs on the CTS website have been updated for the data status
on October 31, 2016, and all transplantations performed until December 31, 2015, with a follow-up of at least
3 months have been included. In these analyses shown on the CTS website, three transplantation periods are
displayed: 1990–2015 and 2000–2015 with a 5-year posttransplant follow-up, and 2008–2015 with a 3-year
posttransplant follow-up.
Please note that only transplantations from centers currently participating in the CTS are included in
the center list attached to this Newsletter or published on the CTS website. As of October 31, 2016, the CTS
database contains 494,473 kidney/pancreas, 75,750 heart/lung and 94,718 liver transplantations with
follow-up.
The next shipping date for the DNA and serum studies is November 14/15, 2016.
Thank you all for your trust and continued support!
Yours sincerely,
Caner Süsal
![]()